London Medical Paediatrics
Paediatric and Adolescent Endocrinology
Here at London Medical, we are dedicated to your child’s total health and well-being. Whether you are looking for ongoing paediatric support or a second opinion from a specialist paediatrician, our world-class consultants deliver care you can trust in a warm and comfortable environment.
What is a paediatric endocrinologist?
A paediatric endocrinologist is a specialist who can accurately test for and treat complex endocrine (hormone) disorders in children and young people. Hormones are responsible for the unconscious processes that control our day-to-day well-being and survival. Hormones regulate your child’s growth and pubertal, reproductive and intellectual development from before birth to maturity (20-25 years). We know it can be distressing for you and your child when maturation doesn’t seem to be progressing as it should. At London Medical, our paediatric endocrinologists offer thorough and holistic clinical assessments to ensure your child receives timely and optimal care that is in their best interests.
Understanding endocrine disorders in children and adolescents
Hormones are chemical messages akin to the body’s ‘letters’. They carry important, instantly-timed information and instructions through the bloodstream to organs and tissues located all over the body and to the body’s glands or ‘post boxes’. There are many hormones, and their interdependency and effects on your child are complex. This highly evolved ‘postal system’ has its control centre — the ‘post office’ — deep in the primitive midbrain. This master gland is called the pituitary gland. It sends and receives a coordinated cascade of messages to and from the other peripheral glands. Together they form the endocrine system.
Hormones must be produced in just the right amounts, at just the right developmental windows of time, and in the right circumstance. Too much or too little of any hormone harms your child’s growth, development and well-being. In some cases, the deficiencies can be life-threatening.
How do hormones affect your child’s health?
Hormones are responsible for controlling and regulating almost every key process in your child’s body, including:
- blood pressure
- body temperature
- sleeping and waking rhythms
- bonding with family (i.e., parents and caregivers)
- thirst sensation
- salt and water balance
- hunger and satiety
- growth and development of the body and brain at four key periods
- energy response to stress and injury (fight-flight)
- thyroid metabolism
- glucose regulation
- bone health and calcium metabolism
- muscle mass
- emotions, mood and behaviour
- onset and progression of puberty
- attainment of reproductive capacity
- female ovulation underpinning a regular menstrual cycle.
These processes are all regulated by the pituitary gland, the primitive ‘control centre’. The pituitary gland can sometimes be maldeveloped or injured. Sometimes one of the other glands in your child’s body might produce too much or too little of a particular hormone. Either can affect the entire balance of the body’s interconnected systems resulting in wide-ranging symptoms. When this happens, your child requires careful and holistic assessment.
When should your child see an endocrinologist?
It can be entirely normal for some children to be much shorter or taller than their peers. Likewise, there is a wide range of normal when it comes to starting puberty. Chronic ill health or undernutrition will delay growth and development.
If you believe your child has abnormally slow or fast growth or are concerned about their weight, your child’s GP or paediatrician should check their growth rates from infancy using the standard growth charts in light of your own (parental) heights. If your child’s growth and development is unusual, they might refer you to a paediatric endocrinologist who can evaluate your child to determine if a hormonal problem is the reason.
Signs and symptoms of an endocrine problem in your child might include:
- excessively short stature
- abnormally tall height
- inappropriate change in growth rate (too slow or too fast for their age)
- obesity
- being underweight
- early puberty (precocious puberty)
- late puberty
- absent, irregular or infrequent periods
- acne
- striae
- excessive body hair (hirsutism)
- excessive hair loss
- excessive thirst or urination (especially during the night)
- excess of sleep (disturbed sleep-wake cycle)
- problems regulating body temperature
- enlarged thyroid glands (goitre)
- excess, unusual fatigue and low energy (which can also be a sign of low mood)
- hyperactivity, palpitations, sweating
What are the conditions that we treat?
Our paediatric endocrinologists can diagnose and treat a wide range of hormonal disorders for children, adolescents and young people up to 20-25 years.
Abnormal growth disorders
If your child appears to have a problem with their height, weight or sexual maturity, it might be a sign of a growth or pubertal delay/disorder. Conditions we treat include:
- Short stature – There are many reasons your child might be below average height for their age and sex, including family predisposition, underlying chronic disease, growth hormone deficiency and genetic conditions which result in an abnormal skeleton.
- Delayed puberty – If a teenage girl has not experienced any breast budding and its accompanying growth spurt by age 13 or had her first period by age 15, she has delayed puberty and needs assessment. Boys have delayed puberty if they have not experienced any pubic hair or testicular enlargement by age 14.
- Early puberty – Also called precocious puberty, this is when your child enters puberty unusually early. For girls, this is when they develop breasts before age 8 or get their first period before 10. For boys, this means pubic hair development and testicular enlargement before age 9.
- Gigantism – This rare condition causes your child to grow abnormally tall due to an overproduction of growth hormone caused by a tumour. There are other syndromes associated with tall stature, the most common of which is overfeeding and obesity from infancy.
Thyroid disorders
The thyroid gland produces the hormones responsible for regulating our metabolic rate, which in turn affect growth, weight, energy levels, body temperature, heart rate, kidney function and blood pressure, as well as our intellectual function. (This is why all babies are screened for thyroid deficiency at birth). Our specialists can treat:
- Hypothyroidism – This condition is when the thyroid gland is absent, maldeveloped, malfunctioning or underactive. Outside infancy, this is generally due to a hereditable tendency to autoimmune disease. When your child’s thyroid levels fall significantly, it could cause weight gain, poor growth and delayed puberty, slower heart rate, constipation, reduced reaction time, inactivity and placidity. Another sign might be lower academic performance.
- Hyperthyroidism – If your child’s thyroid gland is overactive, you might notice symptoms of hyperactivity and increased metabolic rate, such as excess hunger associated with weight loss (and sometimes weight gain), diarrhoea, anxiety, palpitations, fast heart rate, sweaty and trembling hands, problems sleeping, missed periods, exhaustion and changes in school academic performance.
- Goitre – An enlarged thyroid gland will cause noticeable swelling in your child’s neck, evident on swallowing. If it grows very large, it can obstruct breathing and swallowing.
Parathyroid disorders
Parathyroid gland disorders are very rare in childhood but can arise from congenital disorders. Problems with the parathyroid glands can cause disturbances in calcium and bone metabolism from the newborn period and require specialist blood, urine and bone investigations and assessments.
Hypothalamo-Pituitary disorders
The pituitary gland, together with the hypothalamus, is often called the ‘conductor of the endocrine orchestra.’ When the pituitary gland is damaged or doesn’t function properly (e.g., because of damage to the hypothalamus), it can cause severe life-threatening repercussions to many vital functions, including metabolic control (salt, water and glucose balance), childhood growth and development, fight-flight stress response and reproductive functioning.
- Hypothalamo-Pituitary tumours – Although rare in children, tumours of the pituitary gland and in the hypothalamus and visual pathways can disrupt your child’s hormonal balance by causing too much or too little of a particular hormone to be produced at time-inappropriate developmental windows. They can have damaging effects on your child’s vision, or they might present with weight and growth disorders.
- Hypopituitarism – This rare disorder causes your child’s pituitary to underproduce one or more hormones. When all the pituitary hormones are underproduced or absent, this is called panhypopituitarism and is a potentially life-threatening disorder. If children lack one or more hormones, a number of endocrinological conditions, including short stature, delayed puberty, hypothyroidism or adrenal insufficiency, can result.
- Pituitary diabetes insipidus – Not to be confused with diabetes mellitus, which involves high blood sugar levels, diabetes insipidus is a disorder in which the kidneys cannot balance fluids in the body. It is characterised by excessive thirst and urination, particularly at night.
- Craniopharyngiomas – These are rare, slow-growing developmental tumours which are the most common type of pituitary tumour found during childhood. They do not produce hormones but have an invasive capacity to destroy cells that produce pituitary hormones, affecting growth and development and threatening nearby visual pathways in infants and young children.
- Prolactinoma – Although rare in children, prolactinomas are the most common form of pituitary tumour after 15 years of age. These tumours may be the first sign of a familial/genetic disposition in children. They can arise in both adolescent boys and girls, causing an overproduction of prolactin, the hormone responsible for breast milk production. Delayed puberty, headaches or vision problems can result in either sex, but post-pubertal girls, like adult women, may experience early symptoms of irregular periods or a milky breast discharge.
- Gigantism / Acromegaly – This is another overproducing and genetically predisposed pituitary tumour that results in the overproduction of growth hormone. It results in excessively fast growth, tall stature and often delayed puberty. In the growing child, it can cause secondary diabetes mellitus, headaches and visual symptoms.
- Cushing’s syndrome – This condition results from an overproduction of cortisol, causing excess central weight gain, slow growth, abnormal and precocious puberty, evidence of androgen excess (acne, hirsutism, menstrual irregularity, virilisation), high blood pressure and secondary diabetes mellitus. It is typically caused by tiny tumours of the pituitary gland – when it is referred to as Cushing’s Disease – or, more rarely, tumours of the adrenal gland.
Adrenal disorders
Our adrenal glands release the hormones cortisol, adrenaline, and aldosterone, as well as many intermediate ‘steroids’ and weak male hormones (adrenal androgens) in a complex cascade. These hormones are essential for our healthy daily life, including regulating the body’s ‘fight or flight’ response, blood pressure, blood sugar, salt metabolism, fluid balance, heart rate, immunity and healing capacity. A specialist analysis of a 24-hour urine collection can be very informative in diagnosing adrenal disorders.
- Adrenal insufficiency – This condition can result from the destruction of the adrenal gland by haemorrhage, an autoimmune disease called Addison’s Disease or from a loss of pituitary function control (ACTH deficiency). It can also result from temporary but prolonged suppression of the adrenal glands by glucocorticoid steroids, which are prescribed to treat severe chronic diseases such as asthma, arthritis, nephritis and autoimmunity. All forms of adrenal insufficiency are life-threatening and require a programme to replace cortisol both with and without aldosterone.
- Congenital adrenal hyperplasia (CAH) – This adrenal insufficiency genetic disorder is often first diagnosed at birth if severe or later in childhood if it takes a milder form. It most commonly results in excess androgenic steroids (which can virilise a girl) and critical insufficiency of aldosterone and cortisol production.
Our approach to paediatric and adolescent endocrinology
When you’re worried about your child’s health, you don’t want to wait for answers. At London Medical, appointments are booked promptly, blood tests can be done on the same day in-house and results are emailed directly to your consultant, who can share them with you without delay. Our paediatric endocrinologists are considered the top in their field, and they offer personalised care tailored to your child’s individual needs.
Because hormone disorders problems can cause significant mental and psychosocial stress for children and teens, we often suggest that your child sees one of London Medical’s paediatric counsellors for additional support.
Getting diagnosed
Many glandular hormone disorders can be diagnosed with standard blood hormone tests and/or a carefully collected and analysed 24-hour urine collection. Hypothalamo-pituitary disorders in growing children often require more lengthy, dynamic stimulation tests under standardised conditions. Our expert paediatric nurses and lab technicians ensure all blood tests are done safely, effectively and swiftly, protocolised and “packaged” for cost-efficiency.
Your consultant might recommend one or more of the following investigations:
- Basal pituitary hormone blood tests
- Basal hormone tumour markers to screen for occult hormone-producing tumours
- Spot urine tests and 24-hour urine collection for cortisol and steroid analysis, kidney function, puberty and adrenal disorders
- General blood tests and autoimmune screening for chronic diseases
- Fasting glucose cholesterol and lipids to assess secondary diabetes risk
- Vitamin levels for optimal health and well-being
- A stimulation test to measure growth hormone and cortisol secretion
- A stimulation test to assess delayed or precocious puberty
- A glucose tolerance test to assess insulin response to obesity and growth hormone excess
- A water deprivation test to evaluate the possibility of diabetes insipidus
- X-rays of bone age and skeleton to determine height prediction and assess skeletal disorders
- DEXA bone density scan to assess bone mineral accretion and osteoporosis risk
- Specific MRI scans to check the hypothalamus and the pituitary gland’s position, shape and size
- Pelvic ultrasound to assess puberty stage and internal gonadal anatomy
- Thyroid ultrasound and isotope scan to assess thyroid disorders
- Genetic tests to assess genetics of obesity, short stature, pubertal anomalies, pituitary or adrenal tumours, and gonadal, bone and adrenal disorders.
Treatments
Your consultant will advise you on whether treatment is necessary. Often your child might not need any special treatment other than careful clinical monitoring of growth and puberty along a growth centile chart.
If your child has a proven hormone deficiency, replacement hormone therapy can restore normality. This may be in the form of tablets taken in different dose regimens throughout the day. If your child has adrenal insufficiency or diabetes insipidus, you will be advised on the specific emergency protocol in the event of illness, unconsciousness or elective surgery.
Our consultants, together with one of our endocrine nurse specialists, will train you (and your child as they mature) to understand the emergency regimen, notify London ambulance services, and administer an emergency hydrocortisone injection. Our nurses will also train you to administer any daily growth hormone or insulin injections, whereas weekly or monthly intramuscular injections are done in the clinic. Most other replacement medications are available orally or transdermally.
When an excess of hormone is found, treatment depends on identifying the underlying cause.
In cases of thyroid hormone excess, this usually requires oral antithyroid medication.
In abnormal or precocious puberty, this usually involves blocking excess or premature production of sex steroids or balancing replacement of the adrenal deficiency underlying the hormone imbalance.
In the rare cases of a pituitary, adrenal, gonadal or thyroid tumour responsible for excess hormone production, your consultant might suggest one or more of the following initial treatments:
- oral dopamine agonists to reduce prolactin
- injectable anti-growth hormone agents
- genetics to ascertain a predisposing familial cause
- surgery to remove the tumour.
If your child has a tumour, their therapy will always be decided and undertaken in conjunction with the specialist paediatric oncology multidisciplinary treatment centre at Great Ormond Street Hospital.
If your consultant suggests treatment for delayed puberty, they might prescribe a course of low-dose oestrogen for girls or low-dose testosterone for boys to kickstart puberty. In the case of precocious puberty, your consultant might suggest regular puberty-blocking injections that stop the production of the hormones that cause puberty. Sometimes a watch-and-wait strategy is enough to monitor progress.
Whatever the recommended treatment, careful monitoring and follow-up are often recommended. Children taking hormone injections need frequent monitoring of their hormone levels. Holistic paediatric care can help restore and maintain hormonal balance, good health and emotional well-being.
Supporting the transition to adulthood
When the time is right, children with chronic conditions will need to transition from paediatric to adult care. Many paediatric clinics focus on the importance of your child’s transition — this is the time in an adolescent’s life when they move from paediatric care to adult care, often at a set age or cut-off time. Although this specific transition period from paediatric to adult care is important, we believe there is so much more to it than this.
Our growth and development don’t stop just because we become of legal age or move out of our family home. For young people, growth and development, including brain maturity and bone density, continue under the influence of sex hormones until the age of 25, with each individual reaching their full maturity at a time that is unique to them. Our consultants understand this varies for each individual young person and depends on their condition and any co-existing health problems. Our consultants continue to treat their patients beyond the traditional transition time of 16-18 years until the young person is ready to move on.
Whether your child moves out of paediatric care when they are 18 or 25, you can be sure that their paediatric consultant has carefully considered their readiness and made a complete plan with them and you for their successful transition to adult care.
Meet our paediatric endocrinologists
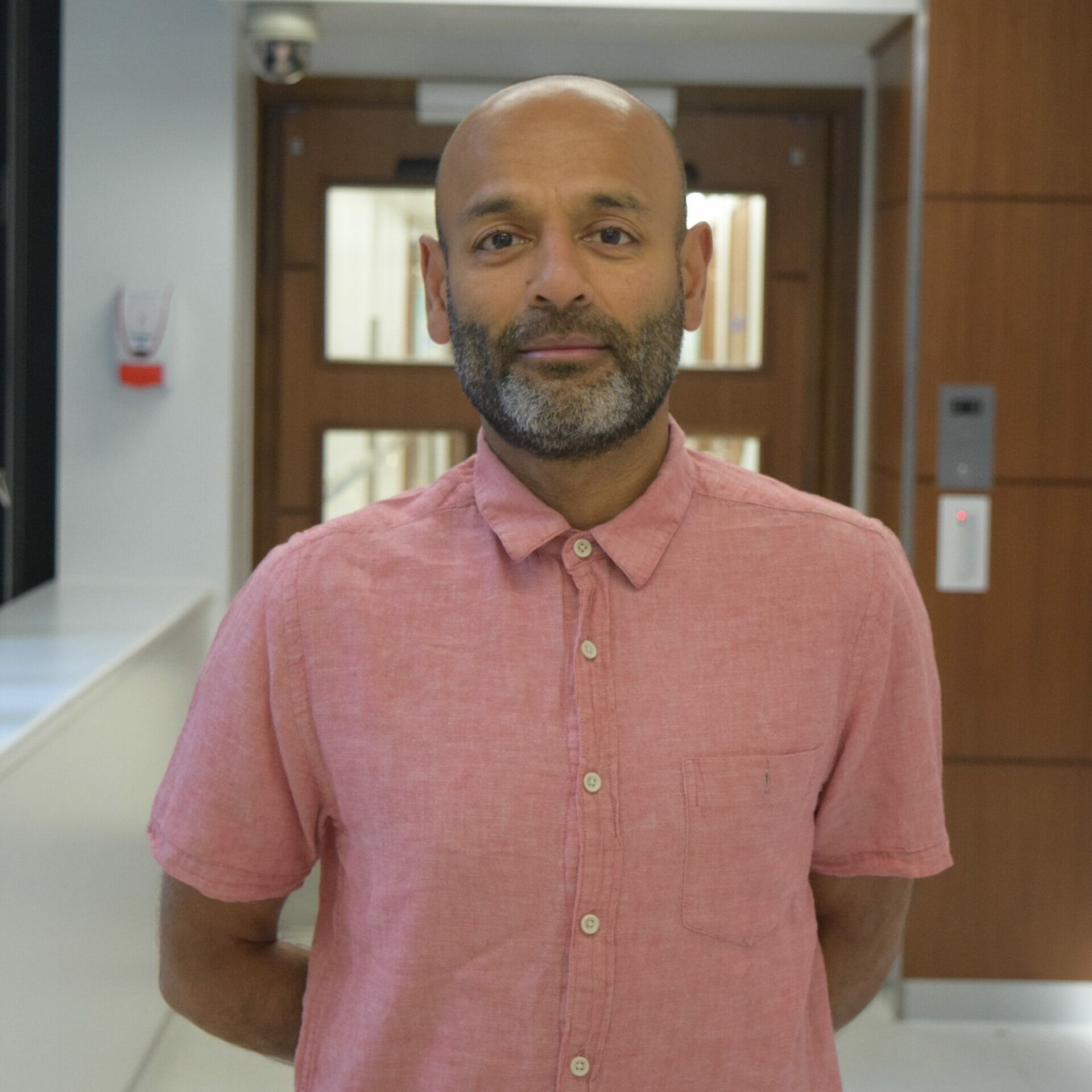
Dr Rakesh Amin
Clinical lead for endocrinology and diabetes at Great Ormond Street Hospital. As a paediatrician, he treats patients aged between 0-25 years of age only.
Dr Martha Ford-Adams
Consultant paediatrician with specialist interest in treating diabetes for children and adolescents.
Professor Stephen Greene
Specialist in child health with positions in Oxford, Great Ormond Street and Guy’s Hospital, London and the Kinderspital Hospital, Zurich.
Our Paediatric specialties
We offer specialist treatment across a wide spectrum of common childhood illnesses and complex chronic conditions.
Explore our paediatric specialties:
Our Locations
London Medical is located in the Harley Street medical area. Together with top experts across a range of multi-disciplinary fields, we offer the finest facilities for your care, all under one roof.
Monday to Friday 8.30am to 8pm
Sundays - 9.00am to 2.00pm
Monday to Friday 8.30am to 8pm
Sundays - 9.00am to 2.0pm
Monday to Friday 8.30am to 8pm
Speak to a member of our team
Contact the appointments team
Make an enquiry online using this form and one of our team will be in touch. By using this form you agree with the storage and handling of your data by our team. Alternatively, you can contact us.
You don't need a referral from your GP to make an appointment with us.
Heart Health News
Find out the latest news, thinking and insights from our experts. Our Heart Health News is your go-to source of trusted advice and knowledge on all matters of the heart.